Treatment at Hamilton Physio & Rehab after a piriformis injection can begin as soon as your doctor allows it. Each doctor will set their own time frames for beginning therapy based on their personal experience, and also based on how your body has reacted to the injection.
If the injection has relieved some or all of your discomfort then, if possible, it is useful to begin treatment at Hamilton Physio & Rehab during the period where you are in less pain. This time frame allows your physiotherapist to take advantage of the pain-free period to stretch your piriformis muscle and to set you up on an individualized home exercise program of stretching and strengthening.
In order to help lengthen and relax a tight or contracted piriformis muscle your therapist may use hands on massage or stretching techniques as well as warm hot packs and electrical modalities such as ultrasound, interferential current, or electrical muscle stimulation. In some cases of lingering pain, ice may also be useful. If your therapist practices a type of needling, such as acupuncture or intramuscular stimulation, then they may also use this technique to assist with your pain and to help release any muscle tension.
Your physiotherapist will prescribe a series of stretching exercises for your hip, buttocks, thigh, low back and, if necessary, your calf. They will also assess the motion of your hip joint. Any tightness in the muscles around the hip and knee or restricted motion in the hip joint itself can affect the biomechanics of the trunk and lower limb, including the tension in the piriformis muscle, so this will need to be addressed. In particular your therapist will encourage you to specifically stretch your piriformis muscle by sitting in a chair or on the ground and crossing the ankle of your affected side over your other knee. By applying gentle pressure downwards on the inside of your thigh of the affected side, while simultaneously sitting up tall (gently tilting your pelvis forward) you will be stretching your piriformis. Your therapist can advise you depending on your individual situation about how often you should be stretching your piriformis muscle and for how long you should hold each stretch. In general doing a long, steady hold of the piriformis stretch will improve flexibility of the piriformis muscle as well as improve the external rotation motion at your hip.
The cause of the initial spasm of your piriformis muscle will need to be investigated by your therapist. In order to assess this they will want to look at your overall posture in standing and sitting and may ask you to do activities like walk, jump, go up or down stairs, or squat on one leg in order to determine your particular pattern of motion and to assess which muscles may be weak or overbearing. In particular the alignment of your pelvis and lower limb will be assessed. Your hip joint, including the piriformis muscle along with the deep gluteal muscles, help to control the position of your lower limb as well as your pelvis. If your muscles are tight or weak they can alter your alignment and biomechanics and if your biomechanics or alignment are off, this can affect the tension in your piriformis muscle.
Your physiotherapist will also assess the motion in your lumbar spine and pelvis as well as the ability of your core muscles to control the trunk. Due to the close proximity of the piriformis muscle to the low back area as well as the relation of the spinal nerves leaving the low back and then forming the large sciatic nerve (which, as explained above, passes near or through the piriformis muscle) this area needs to closely be assessed for its contribution to your dysfunction in the piriformis muscle. If your low back is stiff or degenerating at the joints this can irritate the nerves in the low back or alter the biomechanics of the spine causing the piriformis muscle to become tight. Alternatively a loose (hypermobile) low back joint can also alter the biomechanics of the low back and trunk causing the piriformis to tighten. Often by changing the overall biomechanics of the trunk and lower extremities the piriformis muscle is relieved of excess strain and your pain eases. You therapist will provide advice regarding your individual biomechanics and how you can improve them in your daily activities of work and play.
Having a weak core muscle area can have a similar effect on the lumbar and trunk biomechanics as a stiff or loose lumbar spine and can also lead to pain in the piriformis muscle. Core-strengthening exercises will be crucial to your rehabilitation after a piriformis injection. Your therapist may start these exercises by first just teaching you how to activate the deep muscles that support the spine and trunk. This is done by gently pulling the muscles inwards as you sit or lie on the bed. Pain and injury can make these muscles much less effective and difficult to activate so learning to use them may not be easy at first; the feedback from your physiotherapist regarding technique will be crucial.
As you improve in your control of your core muscles then more difficult exercises such as ones where you are moving your arms or legs while you keep your trunk steady, will be prescribed in order to challenge this area. Lastly, improving the endurance of your core area will be of focus.
Generally the rehabilitation we provide at Hamilton Physio & Rehab after piriformis injections goes very well. If, however, your therapy is not progressing as your therapist believes it should, we may send you back to your doctor for another consult regarding further management of your pain. It is important to remember, however, that injections are not usually a cure for your pain; they are only a part of your overall pain management plan.
Hamilton Physio & Rehab provides services for physiotherapy in Hamilton downtown.
 Piriformis muscle injections are commonly used to determine what is causing buttock and sciatica type pain. Piriformis muscle injections are both diagnostic injections and therapeutic injections, meaning that they can both help your health care professional determine the cause of your pain and may also provide you with relief from the pain. These injections work to eliminate pain temporarily by paralyzing the piriformis muscle and stopping spasm in the muscle. If the piriformis muscle is injected and your pain goes away for several days, then it is very likely that a portion of your pain is caused by piriformis syndrome. Once you and your health care professional know what structure is causing your pain, you can begin to explore options for treating the condition.
Piriformis muscle injections are commonly used to determine what is causing buttock and sciatica type pain. Piriformis muscle injections are both diagnostic injections and therapeutic injections, meaning that they can both help your health care professional determine the cause of your pain and may also provide you with relief from the pain. These injections work to eliminate pain temporarily by paralyzing the piriformis muscle and stopping spasm in the muscle. If the piriformis muscle is injected and your pain goes away for several days, then it is very likely that a portion of your pain is caused by piriformis syndrome. Once you and your health care professional know what structure is causing your pain, you can begin to explore options for treating the condition.
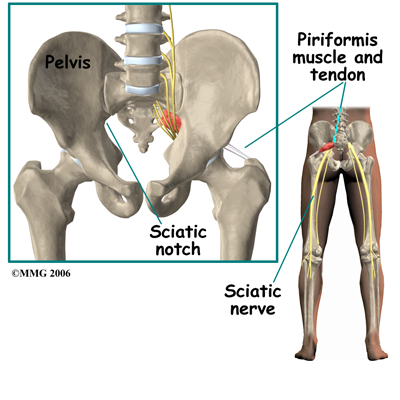
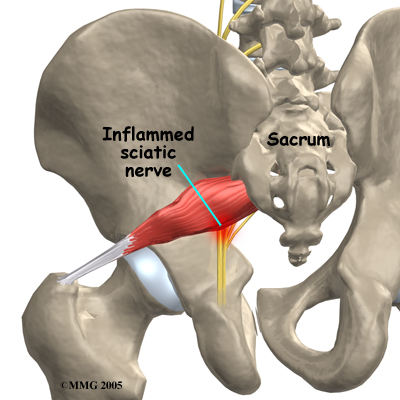
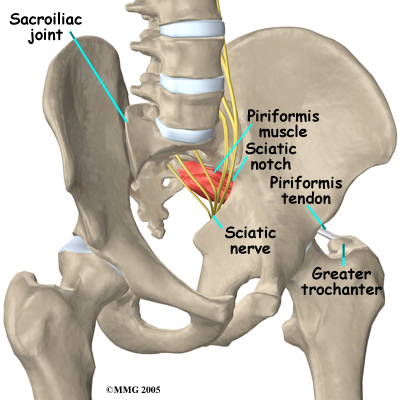 The piriformis muscle is one of the external rotators of the hip and leg. This means that as the muscle works, it helps to turn the foot and leg outwards when you are standing. The piriformis muscle can cause problems when spasm of the muscle irritates one of the large nerves innervating the leg, the sciatic nerve. The sciatic nerve is made up of the lower lumbar and sacral spinal nerves, which leave the spine and join to form the sciatic nerve. The sciatic nerve leaves the pelvis through an opening called the sciatic notch. The sciatic nerve runs under (and in some people through) the piriformis muscle on its way out of the pelvis. Tightness or spasm in this muscle can sometimes cause pain in the area of the muscle, or pain down the back of thigh in the area where the sciatic nerve innervates.
The piriformis muscle is one of the external rotators of the hip and leg. This means that as the muscle works, it helps to turn the foot and leg outwards when you are standing. The piriformis muscle can cause problems when spasm of the muscle irritates one of the large nerves innervating the leg, the sciatic nerve. The sciatic nerve is made up of the lower lumbar and sacral spinal nerves, which leave the spine and join to form the sciatic nerve. The sciatic nerve leaves the pelvis through an opening called the sciatic notch. The sciatic nerve runs under (and in some people through) the piriformis muscle on its way out of the pelvis. Tightness or spasm in this muscle can sometimes cause pain in the area of the muscle, or pain down the back of thigh in the area where the sciatic nerve innervates.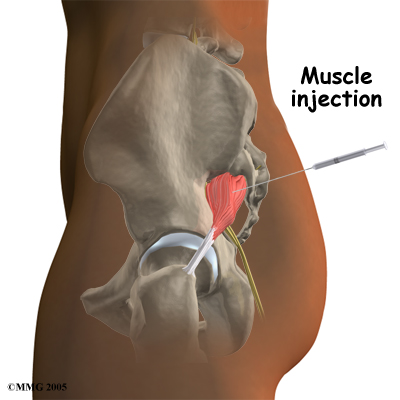
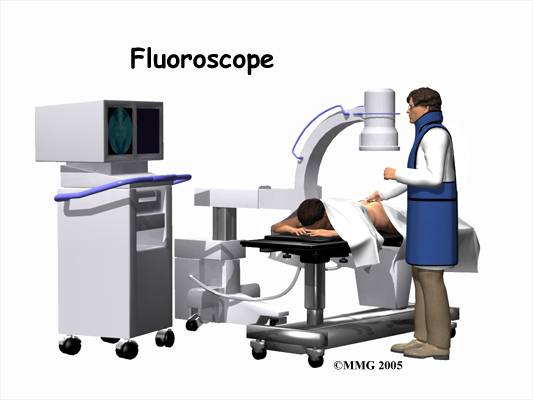 Piriformis muscle injections are done with the help of fluoroscopic guidance. The fluoroscope is an x-ray machine that allows the doctor to actually see an x-ray image while doing the procedure. This allows the doctor to watch where the needle goes as it is inserted. This makes the injection much safer and much more accurate. Once the needle is in the right location, a small amount of radiographic dye is injected. This liquid dye shows up on the x-ray image and the doctor can watch where it goes. The medication used for the injection will go in the same place, so the doctor wants to make sure that the medication goes to the best place to do the most good. Once the correct position is confirmed, the medication is injected and the needle is removed.
Piriformis muscle injections are done with the help of fluoroscopic guidance. The fluoroscope is an x-ray machine that allows the doctor to actually see an x-ray image while doing the procedure. This allows the doctor to watch where the needle goes as it is inserted. This makes the injection much safer and much more accurate. Once the needle is in the right location, a small amount of radiographic dye is injected. This liquid dye shows up on the x-ray image and the doctor can watch where it goes. The medication used for the injection will go in the same place, so the doctor wants to make sure that the medication goes to the best place to do the most good. Once the correct position is confirmed, the medication is injected and the needle is removed.